Lead singer is CanadianLike we should listen to a bunch of geriatric Brit rockers. . .
Oh, wait. It's you. Carry on.
COVID-19 'Pandemic'
- Thread starter Ocean Breeze
- Start date
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
*Plants tongue firmly in cheek*Set it free! Weak mutations are a blessing.
Half a continent is barely far enough.You keep away from my butt cheeks there pupsik.
Money in the bank.It's odd how they can DNA the virus in each and every positive but refuse to test covid survivors for immunity so they can avoid shots and keep their jobs.
FIFY.They, Israel, Hong Kong...
I'll wait to see what other doctors that agree with me say about it first. As it's a new variant other specialists haven't looked into it yet and it'll take weeks before they know the real effect this has. From what I understood at the time I posted, the last I heard was that no one was certain about the extent of the danger it has.
But yet they have the time and resources to identify a one in a million alleged variant in several locations around the globe.
Go figure.
They identified it sure.
Supposedly it's been a thing world wide since October.
That doesn't mean they know the ins and outs of it yet.
Why you're only paying part attention is beyond me, except the fact you're an idiot, so I shouldn't expect much.
Hey, if you want to be ignorant still of facts, that's on you.FIFY.
Saying I want to wait for others outside of South Africa to study it and determine what this new variant is, isn't wrong. It's only smart.
Is it more transmissable? Is it worse? Is it 'lighter' in symptoms? Will it bypass the vaccine? Can the vaccine tackle it? Considering the immediate thoughts that it is easier to transmit - since it was only found in October and is already all over the place - and the other boxes it could tick off, it is something to be wary of.
Now YOU on the other hand, needing doctors to agree with you that it's not that bad and go about your business and whatnot... that's your deal.
Because South African doctors aren’t up to western standards , despite them doing the worlds first heart transplant .They, Israel, Hong Kong...
I'll wait to see what other doctors outside of SA say about it first. As it's a new variant other specialists haven't looked into it yet and it'll take weeks before they know the real effect this has. From what I understood at the time I posted, the last I heard was that no one was certain about the extent of the danger it has.
Give it up, Serryah.Hey, if you want to be ignorant still of facts, that's on you.
Saying I want to wait for others outside of South Africa to study it and determine what this new variant is, isn't wrong. It's only smart.
Is it more transmissable? Is it worse? Is it 'lighter' in symptoms? Will it bypass the vaccine? Can the vaccine tackle it? Considering the immediate thoughts that it is easier to transmit - since it was only found in October and is already all over the place - and the other boxes it could tick off, it is something to be wary of.
Now YOU on the other hand, needing doctors to agree with you that it's not that bad and go about your business and whatnot... that's your deal.
Facts don't help. People willing to admit their ignorance and seek understanding pay attention to facts.
People who just got an ax to grind cherry-pick facts to "prove" their preselected Troof.
3 new COVID-19 cases announced in Ontario
https://globalnews.ca/news/6613790/...erNational&utm_medium=Email&utm_campaign=2020
I am so scared. LOL.
Re: COVIDD-19 'Pandemic'
Flu kills many thousands each year in the UK. See page 51 of this report.
https://assets.publishing.service.g...ruses_in_the_UK_2018_to_2019-FINAL.pdf#page50
The big pharma globalist ilk needs more zombie buffoons like those two around. They are the reasons why this scamdemic stays alive and well.
Re: COVIDD-19 'Pandemic'
The most dangerous thing about coronavirus is the hysteria
It is the latest phenomenon to fulfil our weird and growing appetite for doom
Ross Clark


Ross Clark
29 February 2020
The Spectator
If you have just cancelled your trip to Venice and ordered your £19.99 surgical face mask from Amazon, how about this for a terrifying vision: by the time we get to April, 50,000 Britons will have succumbed to a combination of infectious disease and adverse weather.
Frightened? If you are, don’t worry: you survived. It was two years ago. In 2017-18 the Office for National Statistics recorded 50,100 ‘excess winter deaths’. The explanation, according to the ONS, was probably ‘the predominant strain of flu, the effectiveness of the influenza vaccine, and below average winter temperatures’.
Coronavirus (Covid-19) is a pretty virulent virus all right, but not in the way you might imagine. It is less our respiratory tracts it has infected than our inner sense of angst. By last Monday there were 79,331 confirmed cases worldwide, all but 2,069 of which were in China. There have been 2,595 deaths in China and 23 elsewhere in the world. And seasonal flu? According to an estimate by the US-based Center for Disease Control and Prevention, it has caused between 291,000 and 646,000 deaths globally a year. To put it another way, if the number of deaths from coronavirus rises a hundredfold in the next few weeks or months, it will only have reached the lower bound of the estimate for existing strains of flu.
How many of us wear face masks because of winter flu? How many planes and trains are cancelled? Does the stock market slump? There is some justification for being more wary of Covid-19 than the flu. The former is an unknown quantity and we don’t yet have a vaccine. But we know more about it by the day. Its death rate is now around 1 per cent or less and it is mostly killing people with pre-existing health conditions; anyone else would be unlucky to die from it.
Coronavirus hysteria occurs because we confuse precaution with risk. We see Chinese cities being cut off, people being quarantined, factories closed, the streets emptying (save for a few people in face masks) and we interpret this as a sign of grave and imminent danger. If China had not taken such dramatic steps to stop the disease, we wouldn’t be half as worried.
There seems to be a distinct strain of Sino-phobia in our attitude towards infectious disease. Every novel disease that comes out of China instantly seems to gain the description ‘pandemic’ — even when diseases such as Sars and H5N1 avian flu hardly justify being called an ‘epidemic’. Covid-19 seems to fit neatly with our fears about Huawei spying on our phones and Chinese manufacturers stealing our jobs. Diseases from elsewhere don’t excite the imagination nearly so much. There was a brief flurry of concern in 2014 when Ebola, vastly more lethal than Covid-19, emerged in West Africa (it has since killed 11,310 people globally). But if we are going to worry about any infectious disease, it ought to be tuberculosis. The World Health Organization reports there were ten million new cases worldwide in 2018, 1.45 million deaths, and 4,672 cases in England. But no one ever bought a face mask because of that. How many people even know that the epicentre of tuberculosis is India, with 27 per cent of cases globally?
There is something more to the Covid-19 panic. It is the latest phenomenon to fulfil a weird and growing appetite for doom among the populations of developed countries. We are living in the healthiest, most peaceful time in history, yet we cannot seem to accept it. We constantly have to invent bogeymen, from climate alarmism, nuclear war and financial collapse to deadly diseases. Covid-19 has achieved such traction because it has emerged at just the right time. At the end of January, Brexit had just been completed without incident. The standoff between the US and Iran — which preposterously led the ‘Doomsday Clock’ to be advanced closer to midnight than during the Cuban missile crisis — fizzled into nothing. The Australian bush fires, which caused an explosion in climate doom-mongering (even though the global incidence of wildfires has fallen over the past two decades) had largely gone out. What more was there to worry about?
Then along came a novel strain of disease and the cycle of panic began again. But there are already strong signs that it has peaked. In the seven days before 24 February, the WHO recorded 6,398 new infections in China — down from 13,002 the previous week. On Monday it was 415. Very soon we are going to have to find another thing to agonise about. Asteroids? The next ‘freak’ weather incident, now the storms have died down? Who knows, but we will certainly find something.
https://www.spectator.co.uk/2020/02/the-most-dangerous-thing-about-coronavirus-is-the-hysteria/
As long as those stunned peasants out there keep allowing themselves to be a bunch of guinea pigs for big pharma, hysteria will remain alive and well forever. They are the fools that keep all of this covid bull chit alive and well. Sadly, there are way too many of those stupid buffoons around.
Ontario reaches 10,000 COVID-related deaths
Author of the article:
Canadian Press
Canadian Press
Publishing date:
Nov 30, 2021 • 10 hours ago • 4 minute read •
90 Comments
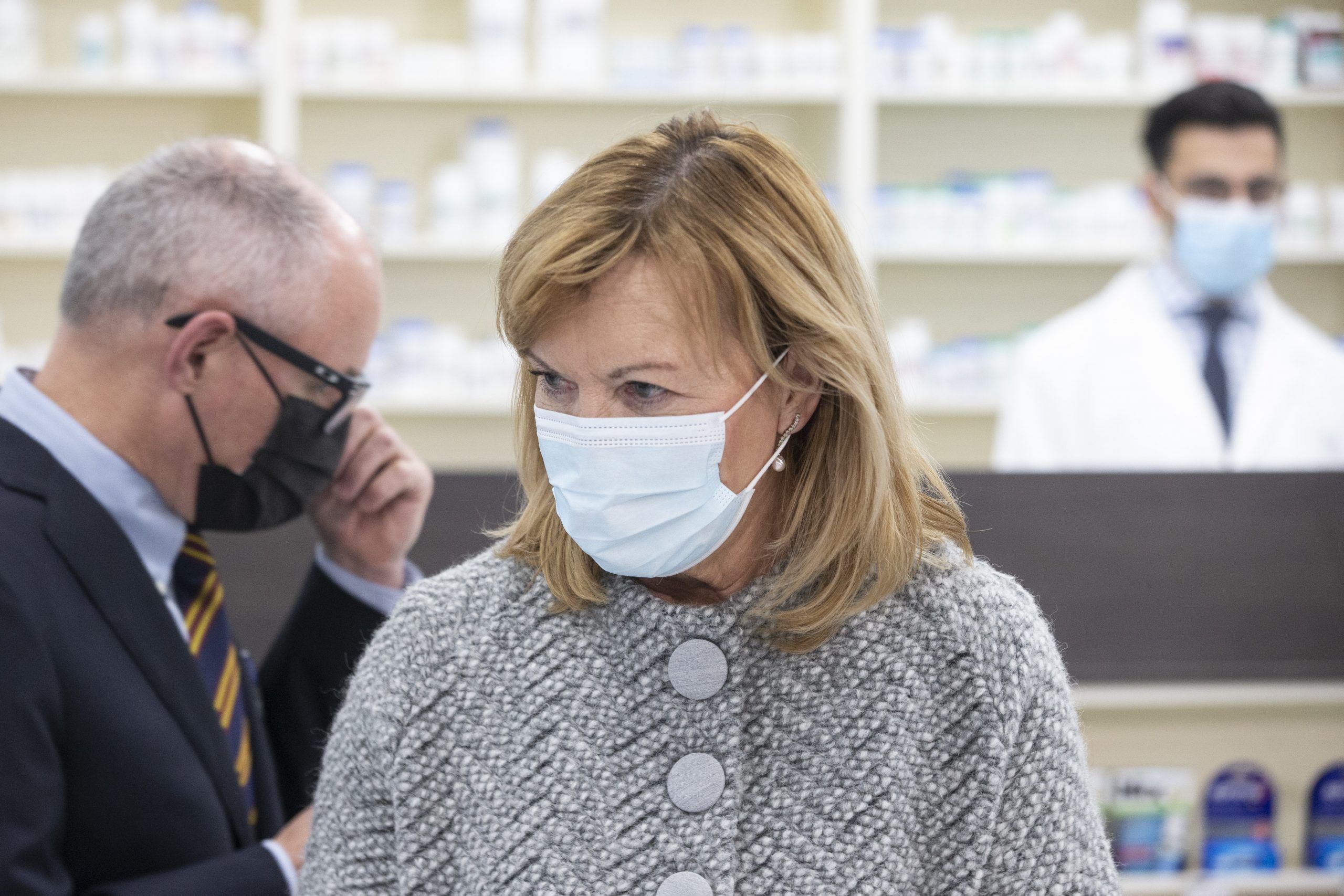
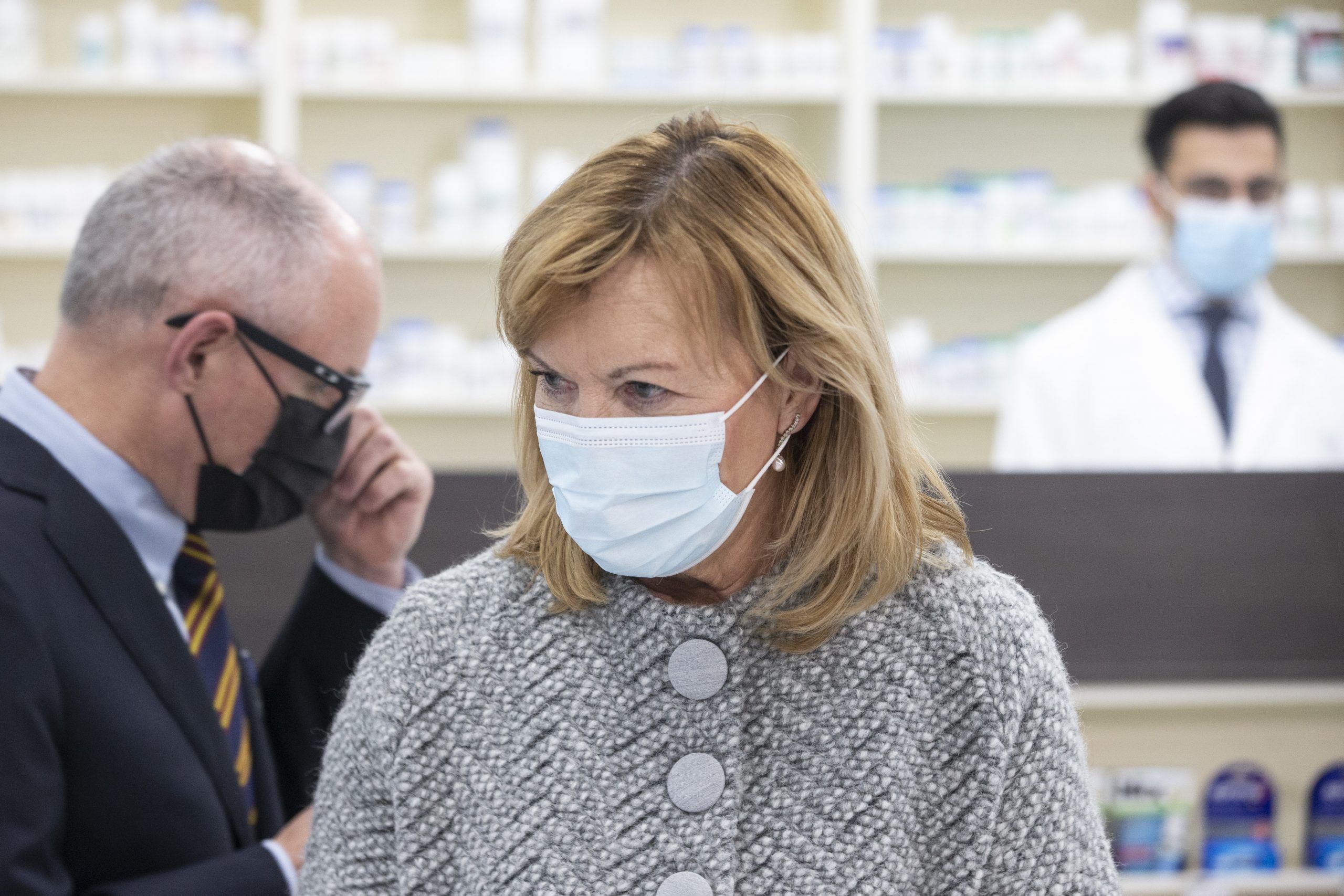
Ontario Health Minister Christine Elliott (centre) trades places at the podium with Dr Kieran Moore (left), Ontario's Chief Medical Officer of Health, at a news conference held in a Toronto pharmacy on Thursday, November 18, 2021.
Ontario Health Minister Christine Elliott (centre) trades places at the podium with Dr Kieran Moore (left), Ontario's Chief Medical Officer of Health, at a news conference held in a Toronto pharmacy on Thursday, November 18, 2021. Photo by Chris Young /THE CANADIAN PRESS
Article content
The only times Sylvia Grady was allowed to see her partner of 22 years as he battled COVID-19 in intensive care was when doctors believed he was on the brink of death — she made that trip three times.
Advertisement
Story continues below
Article content
Those visits to Toronto Western Hospital between April and June last year to say her final goodbyes to Stewart Nanibush felt “otherworldly,” Grady said. He was in an induced coma and unable to reciprocate.
In between those heartbreaking encounters, she was able to call the ICU and staff would hold a phone up to Nanibush.
“I would call every night to say words, you know, just tell him a story, to play a bit of music for him,” she said in an interview, tearing up as she recalled his death.
“I’m 64. I’m no young one ⦠I guess in certain ways I was prepared. But this was a pretty big one.”
Nanibush, who was from Wasauksing First Nation near Parry Sound, Ont., was one of 10,000 people in Ontario who have died of COVID-19. Ontario reported three new deaths Tuesday, pushing the provincial total up to the grim milestone.
Advertisement
Story continues below
Article content
Nanibush was 65 years old. He and Grady fell in love when he did some carpentry work at her beeswax candles and artworks store in Toronto, she said. They would later sell his Indigenous crafts at the store.
He chose not to retire from his job at a community centre when the pandemic started, Grady said. She urged him to stay home but he wouldn’t listen and he contracted the virus — either at work or on transit, Grady believes.
Nanibush had asthma and other health issues that made it hard for him to breathe, but he didn’t want to go to the hospital after he got COVID-19 because of the systemic racism Indigenous people face in the health-care system, Grady said.
After spending a week in bed, Nanibush got very sick.
“On the day he went in, we discussed the ambulance in the morning. He said, ‘No, I don’t want to (go to the hospital)’ and then in the evening, it was clear that he needed to go, so I called the ambulance,” she said.
Advertisement
Story continues below
Article content
“I don’t think I fully recovered from the shock of that day.”
COVID-19 has claimed the lives of Ontarians from all age groups and walks of life, but it has hit older residents hard, with about 5,900 people aged 80 and over dying due to the virus, according to Public Health Ontario data.
The median age of deaths has decreased through each subsequent wave of the pandemic, provincial data shows. From the first wave to the fourth, it dropped from 85 years old to 74.
Long-term care residents have been disproportionately affected, with more than 40 per cent of all deaths in the province occurring in that population.
A report on the latest pandemic projections from the Ontario COVID-19 Science Advisory Table also notes that people with lower incomes, essential workers and visible minorities have experienced the highest risk of COVID-19-related mortality.
Advertisement
Story continues below
Article content
Christine Mandegarian was one of several essential workers who fell victim to the virus.
She worked for 31 years at Altamont Care Community, a long-term care home in east Toronto that was among the many nursing homes devastated by the pandemic.
The upbeat and dedicated personal support worker died just one week before her 55th birthday, on April 15, 2020.
“I was in shock,” recalled Stephaney Williams, who began working alongside Mandegarian at the home in the 1980s.
“I couldn’t believe that we actually lost a coworker to this … It’s a close knit group, so we all got to know her kids, we knew her husband, so it really, really hit home.”
Mandegarian treated her patients and colleagues like her own family, said Williams. She would often bring in homemade Filipino dishes to share and she was adored by staff and patients, Williams said.
Advertisement
Story continues below
Article content
From time to time, Williams thinks about what could’ve gone differently at the long-term care home.
“If they don’t give us the proper PPE, you want to say, ‘OK, we’re not going to do anything until we get what we need,”’ she said, referencing the shortages of personal protective equipment that marked the first wave.
“But then there are vulnerable residents that need us, you know what I mean? So you still have to do your job.”
COVID-19 swept through long-term care homes in the first wave, leaving 1,937 residents dead in those first months – more than 32 per cent of all deaths in the province at that time, according to Public Health Ontario data.
Long-term care homes saw roughly the same number of deaths during the second wave, though by that time the virus was tearing its way through other populations and nursing home deaths represented 21 per cent of the second-wave total.
Advertisement
Story continues below
Article content
Karen Born, the assistant scientific director of the Ontario COVID-19 Science Advisory Table, said in the third wave, there was more infection among essential workers, the people who weren’t able to stay home.
“The essential worker population is a population that is more likely to be from racialized populations and low-income populations as well,” Born added.
Ever since the rollout of vaccines, there’s been a decrease in the number of deaths overall, Born noted. However, those who have not been fully vaccinated are still seeing high rates of infection, hospitalization and death, she said.
At the Altamont long-term care home, the memory of Mandegarian lives on. Williams said a room has been dedicated to her memory and Mandegarian is often thought of by those who knew her.
“Sometimes you’re walking down the hall and you reach a certain area or you go into the staff room – it’s almost like you hear her voice laughing or giving you a joke,” she said. “We think about her a lot.”
 torontosun.com
torontosun.com
Author of the article:
Canadian Press
Canadian Press
Publishing date:
Nov 30, 2021 • 10 hours ago • 4 minute read •
90 Comments
Ontario Health Minister Christine Elliott (centre) trades places at the podium with Dr Kieran Moore (left), Ontario's Chief Medical Officer of Health, at a news conference held in a Toronto pharmacy on Thursday, November 18, 2021.
Ontario Health Minister Christine Elliott (centre) trades places at the podium with Dr Kieran Moore (left), Ontario's Chief Medical Officer of Health, at a news conference held in a Toronto pharmacy on Thursday, November 18, 2021. Photo by Chris Young /THE CANADIAN PRESS
Article content
The only times Sylvia Grady was allowed to see her partner of 22 years as he battled COVID-19 in intensive care was when doctors believed he was on the brink of death — she made that trip three times.
Advertisement
Story continues below
Article content
Those visits to Toronto Western Hospital between April and June last year to say her final goodbyes to Stewart Nanibush felt “otherworldly,” Grady said. He was in an induced coma and unable to reciprocate.
In between those heartbreaking encounters, she was able to call the ICU and staff would hold a phone up to Nanibush.
“I would call every night to say words, you know, just tell him a story, to play a bit of music for him,” she said in an interview, tearing up as she recalled his death.
“I’m 64. I’m no young one ⦠I guess in certain ways I was prepared. But this was a pretty big one.”
Nanibush, who was from Wasauksing First Nation near Parry Sound, Ont., was one of 10,000 people in Ontario who have died of COVID-19. Ontario reported three new deaths Tuesday, pushing the provincial total up to the grim milestone.
Advertisement
Story continues below
Article content
Nanibush was 65 years old. He and Grady fell in love when he did some carpentry work at her beeswax candles and artworks store in Toronto, she said. They would later sell his Indigenous crafts at the store.
He chose not to retire from his job at a community centre when the pandemic started, Grady said. She urged him to stay home but he wouldn’t listen and he contracted the virus — either at work or on transit, Grady believes.
Nanibush had asthma and other health issues that made it hard for him to breathe, but he didn’t want to go to the hospital after he got COVID-19 because of the systemic racism Indigenous people face in the health-care system, Grady said.
After spending a week in bed, Nanibush got very sick.
“On the day he went in, we discussed the ambulance in the morning. He said, ‘No, I don’t want to (go to the hospital)’ and then in the evening, it was clear that he needed to go, so I called the ambulance,” she said.
Advertisement
Story continues below
Article content
“I don’t think I fully recovered from the shock of that day.”
COVID-19 has claimed the lives of Ontarians from all age groups and walks of life, but it has hit older residents hard, with about 5,900 people aged 80 and over dying due to the virus, according to Public Health Ontario data.
The median age of deaths has decreased through each subsequent wave of the pandemic, provincial data shows. From the first wave to the fourth, it dropped from 85 years old to 74.
Long-term care residents have been disproportionately affected, with more than 40 per cent of all deaths in the province occurring in that population.
A report on the latest pandemic projections from the Ontario COVID-19 Science Advisory Table also notes that people with lower incomes, essential workers and visible minorities have experienced the highest risk of COVID-19-related mortality.
Advertisement
Story continues below
Article content
Christine Mandegarian was one of several essential workers who fell victim to the virus.
She worked for 31 years at Altamont Care Community, a long-term care home in east Toronto that was among the many nursing homes devastated by the pandemic.
The upbeat and dedicated personal support worker died just one week before her 55th birthday, on April 15, 2020.
“I was in shock,” recalled Stephaney Williams, who began working alongside Mandegarian at the home in the 1980s.
“I couldn’t believe that we actually lost a coworker to this … It’s a close knit group, so we all got to know her kids, we knew her husband, so it really, really hit home.”
Mandegarian treated her patients and colleagues like her own family, said Williams. She would often bring in homemade Filipino dishes to share and she was adored by staff and patients, Williams said.
Advertisement
Story continues below
Article content
From time to time, Williams thinks about what could’ve gone differently at the long-term care home.
“If they don’t give us the proper PPE, you want to say, ‘OK, we’re not going to do anything until we get what we need,”’ she said, referencing the shortages of personal protective equipment that marked the first wave.
“But then there are vulnerable residents that need us, you know what I mean? So you still have to do your job.”
COVID-19 swept through long-term care homes in the first wave, leaving 1,937 residents dead in those first months – more than 32 per cent of all deaths in the province at that time, according to Public Health Ontario data.
Long-term care homes saw roughly the same number of deaths during the second wave, though by that time the virus was tearing its way through other populations and nursing home deaths represented 21 per cent of the second-wave total.
Advertisement
Story continues below
Article content
Karen Born, the assistant scientific director of the Ontario COVID-19 Science Advisory Table, said in the third wave, there was more infection among essential workers, the people who weren’t able to stay home.
“The essential worker population is a population that is more likely to be from racialized populations and low-income populations as well,” Born added.
Ever since the rollout of vaccines, there’s been a decrease in the number of deaths overall, Born noted. However, those who have not been fully vaccinated are still seeing high rates of infection, hospitalization and death, she said.
At the Altamont long-term care home, the memory of Mandegarian lives on. Williams said a room has been dedicated to her memory and Mandegarian is often thought of by those who knew her.
“Sometimes you’re walking down the hall and you reach a certain area or you go into the staff room – it’s almost like you hear her voice laughing or giving you a joke,” she said. “We think about her a lot.”
Ontario reaches 10,000 COVID-related deaths
The only times Sylvia Grady was allowed to see her partner of 22 years as he battled COVID-19 in intensive care was when doctors believed he was on the brink of dea…
Ontario wrote off $210M in COVID support provided to ineligible businesses: AG
The government has shown no interest in trying to recoup the funds, Lysyk said
Author of the article:
Antonella Artuso
Antonella Artuso
Publishing date:
Dec 01, 2021 • 9 hours ago • 3 minute read •
55 Comments
Bonnie Lysyk, Auditor General of Ontario answers questions during her Annual Report news conference at the Ontario Legislature in Toronto on Monday December 7, 2020.
Bonnie Lysyk, Auditor General of Ontario answers questions during her Annual Report news conference at the Ontario Legislature in Toronto on Monday December 7, 2020. Photo by Frank Gunn /THE CANADIAN PRESS
Article content
A small Ontario business reporting a 0.2 cent loss due to COVID-19 was still able to get $10,000 in taxpayer-funded COVID-19 supports.
Advertisement
Story continues below
Article content
Ontario auditor general Bonnie Lysyk’s annual audit has revealed the Doug Ford government shovelled out almost $1 billion in support overpayments to small businesses that were either ineligible or had asked for less money.
Lysyk said the government has shown no interest in trying to recoup the funds.
Instead, the province wrote off over $210 million provided to about 14,500 ineligible companies through the Ontario Small Business Support Grant.
Another $6 million was paid to 212 “suspicious recipients” that are still being investigated.
And more than 51,000 businesses received $939 million in grants despite reporting only $225 million in losses because the minimum ask was $10,000.
For example, some recipients reported that they lost as little as $0.02 or experienced no change at all in their revenues, yet received $10,000, the report says, adding the overpayment adds up to $714 million.
Advertisement
Story continues below
Article content
Ford said his government doesn’t believe in wasting taxpayers’ money.
“Similar to the federal government, when we’re rushing the money out the door to support the small businesses that were in desperate need of it, unfortunately you’re going to see some fraud,” Ford said. “And we don’t take that lightly … but I think more people benefited than got hurt on that.”
Lysyk said she understands that some money could go to the wrong recipients when the government is in a hurry to provide supports but she’s recommending more care be taken to prevent it.
“It’s a lot of money — $210 million is a lot of money,” Lysyk said.
A spokesperson for Economic Development Minister Vic Fedeli issued a statement insisting the auditor’s numbers on the support program were incorrect, but Lysyk’s office confirmed she stands by her report.
Advertisement
Story continues below
Article content
On health care, the auditors discovered wait times for cardiac procedures grew by 44% over a five-year period, and the number of patients who died on that wait list grew by 42% from 147 in 2015-19 to 209 in 2019-20.
The wait list grew during the pandemic to 8,340 from 7,850 just the prior year.
“The number of people who died while on a wait list for a cardiac procedure also increased by over 10%, from 209 deaths in 2019-20 to 231 in 2020-21,” the report says, adding there is an unknown future cost to treating “missing patients” from the pandemic.
While Ontario’s health-care system matches or exceeds that of other Canadian jurisdictions in preventing death from cardiac and stroke events, provincial treatment-time targets have not been met, the report says.
Advertisement
Story continues below
Article content
However, auditors said hospitals could do a better job in providing timely emergency treatment to avoid permanent damage.
Less invasive treatments are not used enough, the report says.
“We noted that the difference in price that Ontario hospitals pay for the same types of (cardiac) devices can vary by as much as 367%,” the report says. “For example, one hospital was able to procure a simple ablation catheter at an average price of about $300 while another hospital pays an average price of about $1,400 for each simple ablation catheter.”
More On This Topic
Queen's Park in Toronto.
Ontario auditor general annual report's key findings
An Ontario Provincial Police officer uniform
OPP officers' PTSD contributing to staffing shortages: Auditor report
The auditor pointed out the need for more public education on symptoms as 40% of stroke patients did not take an ambulance to hospital and 30% went to a facility that did not specialize in the needed treatment.
Wait times for out-patient surgeries, already high going into the pandemic, have soared since.
According to data from Ontario Health, in 2020-21, almost 350,000 outpatient surgeries were performed in Ontario, compared to approximately 457,000 to 475,000 outpatient surgeries in the four years prior to the impact of COVID-19,” the report says.
aartuso@postmedia.com

 torontosun.com
torontosun.com
The government has shown no interest in trying to recoup the funds, Lysyk said
Author of the article:
Antonella Artuso
Antonella Artuso
Publishing date:
Dec 01, 2021 • 9 hours ago • 3 minute read •
55 Comments
Bonnie Lysyk, Auditor General of Ontario answers questions during her Annual Report news conference at the Ontario Legislature in Toronto on Monday December 7, 2020.
Bonnie Lysyk, Auditor General of Ontario answers questions during her Annual Report news conference at the Ontario Legislature in Toronto on Monday December 7, 2020. Photo by Frank Gunn /THE CANADIAN PRESS
Article content
A small Ontario business reporting a 0.2 cent loss due to COVID-19 was still able to get $10,000 in taxpayer-funded COVID-19 supports.
Advertisement
Story continues below
Article content
Ontario auditor general Bonnie Lysyk’s annual audit has revealed the Doug Ford government shovelled out almost $1 billion in support overpayments to small businesses that were either ineligible or had asked for less money.
Lysyk said the government has shown no interest in trying to recoup the funds.
Instead, the province wrote off over $210 million provided to about 14,500 ineligible companies through the Ontario Small Business Support Grant.
Another $6 million was paid to 212 “suspicious recipients” that are still being investigated.
And more than 51,000 businesses received $939 million in grants despite reporting only $225 million in losses because the minimum ask was $10,000.
For example, some recipients reported that they lost as little as $0.02 or experienced no change at all in their revenues, yet received $10,000, the report says, adding the overpayment adds up to $714 million.
Advertisement
Story continues below
Article content
Ford said his government doesn’t believe in wasting taxpayers’ money.
“Similar to the federal government, when we’re rushing the money out the door to support the small businesses that were in desperate need of it, unfortunately you’re going to see some fraud,” Ford said. “And we don’t take that lightly … but I think more people benefited than got hurt on that.”
Lysyk said she understands that some money could go to the wrong recipients when the government is in a hurry to provide supports but she’s recommending more care be taken to prevent it.
“It’s a lot of money — $210 million is a lot of money,” Lysyk said.
A spokesperson for Economic Development Minister Vic Fedeli issued a statement insisting the auditor’s numbers on the support program were incorrect, but Lysyk’s office confirmed she stands by her report.
Advertisement
Story continues below
Article content
On health care, the auditors discovered wait times for cardiac procedures grew by 44% over a five-year period, and the number of patients who died on that wait list grew by 42% from 147 in 2015-19 to 209 in 2019-20.
The wait list grew during the pandemic to 8,340 from 7,850 just the prior year.
“The number of people who died while on a wait list for a cardiac procedure also increased by over 10%, from 209 deaths in 2019-20 to 231 in 2020-21,” the report says, adding there is an unknown future cost to treating “missing patients” from the pandemic.
While Ontario’s health-care system matches or exceeds that of other Canadian jurisdictions in preventing death from cardiac and stroke events, provincial treatment-time targets have not been met, the report says.
Advertisement
Story continues below
Article content
However, auditors said hospitals could do a better job in providing timely emergency treatment to avoid permanent damage.
Less invasive treatments are not used enough, the report says.
“We noted that the difference in price that Ontario hospitals pay for the same types of (cardiac) devices can vary by as much as 367%,” the report says. “For example, one hospital was able to procure a simple ablation catheter at an average price of about $300 while another hospital pays an average price of about $1,400 for each simple ablation catheter.”
Queen's Park in Toronto.
Ontario auditor general annual report's key findings
An Ontario Provincial Police officer uniform
OPP officers' PTSD contributing to staffing shortages: Auditor report
The auditor pointed out the need for more public education on symptoms as 40% of stroke patients did not take an ambulance to hospital and 30% went to a facility that did not specialize in the needed treatment.
Wait times for out-patient surgeries, already high going into the pandemic, have soared since.
According to data from Ontario Health, in 2020-21, almost 350,000 outpatient surgeries were performed in Ontario, compared to approximately 457,000 to 475,000 outpatient surgeries in the four years prior to the impact of COVID-19,” the report says.
aartuso@postmedia.com

Ontario wrote off $210M in COVID support provided to ineligible businesses: AG
The government has shown no interest in trying to recoup the funds, Lysyk said
BRILLIANT: If COVID Omicron Variant Is as Mild as Indicated Why Not Let It Run Its Course and and Protect Vulnerable with Therapeutics?
By Joe HoftPublished December 2, 2021 at 8:45am
127 Comments
Because they need you to stay home or you'll see empty store shelves for yourself.BRILLIANT: If COVID Omicron Variant Is as Mild as Indicated Why Not Let It Run Its Course and and Protect Vulnerable with Therapeutics?
By Joe Hoft
Published December 2, 2021 at 8:45am
127 Comments
Pfizer begins application for Health Canada's approval of COVID-19 pill
Author of the article:
Reuters
Reuters
Publishing date:
Dec 01, 2021 • 1 day ago • 1 minute read •
Join the conversation
Paxlovid, a Pfizer's coronavirus disease pill, is seen manufactured in Ascoli, Italy, in this undated handout photo obtained by Reuters on Nov. 16, 2021.
Paxlovid, a Pfizer's coronavirus disease pill, is seen manufactured in Ascoli, Italy, in this undated handout photo obtained by Reuters on Nov. 16, 2021. Photo by Pfizer /Handout via REUTERS
Article content
Pfizer Inc said on Wednesday it had started the real-time submission of its application seeking Health Canada’s approval of its oral COVID-19 antiviral drug candidate.
Advertisement
Story continues below
Article content
The pill, PF-07321332, is designed to block a key enzyme needed for the coronavirus to multiply.
The move comes after the Canadian government announced on Tuesday that it was in advanced talks with Pfizer and Merck & Co Inc regarding a purchase agreement for their COVID-19 antiviral drugs, as the country attempts to control the spread of the Omicron coronavirus variant.
The country has identified seven people with the new variant as of Nov. 30.
The drugmaker last month submitted its application seeking U.S. authorization of the experimental pill, which was shown to cut the chance of hospitalization or death for adults at risk of severe disease by 89% in a clinical trial.

 torontosun.com
torontosun.com
Author of the article:
Reuters
Reuters
Publishing date:
Dec 01, 2021 • 1 day ago • 1 minute read •
Join the conversation
Paxlovid, a Pfizer's coronavirus disease pill, is seen manufactured in Ascoli, Italy, in this undated handout photo obtained by Reuters on Nov. 16, 2021.
Paxlovid, a Pfizer's coronavirus disease pill, is seen manufactured in Ascoli, Italy, in this undated handout photo obtained by Reuters on Nov. 16, 2021. Photo by Pfizer /Handout via REUTERS
Article content
Pfizer Inc said on Wednesday it had started the real-time submission of its application seeking Health Canada’s approval of its oral COVID-19 antiviral drug candidate.
Advertisement
Story continues below
Article content
The pill, PF-07321332, is designed to block a key enzyme needed for the coronavirus to multiply.
The move comes after the Canadian government announced on Tuesday that it was in advanced talks with Pfizer and Merck & Co Inc regarding a purchase agreement for their COVID-19 antiviral drugs, as the country attempts to control the spread of the Omicron coronavirus variant.
The country has identified seven people with the new variant as of Nov. 30.
The drugmaker last month submitted its application seeking U.S. authorization of the experimental pill, which was shown to cut the chance of hospitalization or death for adults at risk of severe disease by 89% in a clinical trial.

Pfizer begins application for Health Canada's approval of COVID-19 pill
Pfizer Inc said on Wednesday it had started the real-time submission of its application seeking Health Canada’s approval of its oral COVID-19 antiviral drug candida…
COVID-19 shows up in Canadian wildlife for first time with three Quebec deer infected
Author of the article:
Canadian Press
Canadian Press
Publishing date:
Dec 01, 2021 • 1 day ago • 1 minute read •
7 Comments
A deer is seen at the Michel-Chartrand Park in Longueuil, Que., Friday, Nov. 13, 2020.
A deer is seen at the Michel-Chartrand Park in Longueuil, Que., Friday, Nov. 13, 2020. Photo by Paul Chiasson /THE CANADIAN PRESS
Article content
OTTAWA — For the first time, the COVID-19 virus has been detected in Canadian wildlife.
Advertisement
Story continues below
Article content
Environment Canada says the virus was detected late last month in three wild white-tailed deer in Quebec.
The department says the deer all appeared healthy and showed no clinical signs of COVID-19.
The discovery follows recent reports of the virus spreading among white-tailed deer in the United States.
There has so far been no known transmission of COVID-19 from deer to humans and Environment Canada says it remains “largely a disease of human concern and typically spreads from human to human.”
Still, until more is known, it says anyone exposed to respiratory tissues and fluids from deer should wear a well-fitting mask and avoid splashing of fluids as much as possible.
COVID-19 has infected multiple species of animals, including dogs, cats, farmed mink and zoo animals. But this is the first time in Canada that it has spilled over into wildlife.
Advertisement
Story continues below
Article content
Deer in the Estrie region of Quebec were sampled Nov. 6 to 8. The National Centre for Foreign Animal Disease confirmed the virus in three of them on Monday. The World Organisation for Animal Health was notified on Wednesday.
“As this is the first detection of SARS-CoV-2 in wildlife in Canada, information on the impacts and spread of the virus in wild deer populations is currently limited,” Environment Canada said in a news release Wednesday.
“This finding emphasizes the importance of ongoing surveillance for SARS-CoV-2 in wildlife to increase our understanding about SARS-CoV-2 on the human-animal interface.”

 torontosun.com
torontosun.com
Author of the article:
Canadian Press
Canadian Press
Publishing date:
Dec 01, 2021 • 1 day ago • 1 minute read •
7 Comments
A deer is seen at the Michel-Chartrand Park in Longueuil, Que., Friday, Nov. 13, 2020.
A deer is seen at the Michel-Chartrand Park in Longueuil, Que., Friday, Nov. 13, 2020. Photo by Paul Chiasson /THE CANADIAN PRESS
Article content
OTTAWA — For the first time, the COVID-19 virus has been detected in Canadian wildlife.
Advertisement
Story continues below
Article content
Environment Canada says the virus was detected late last month in three wild white-tailed deer in Quebec.
The department says the deer all appeared healthy and showed no clinical signs of COVID-19.
The discovery follows recent reports of the virus spreading among white-tailed deer in the United States.
There has so far been no known transmission of COVID-19 from deer to humans and Environment Canada says it remains “largely a disease of human concern and typically spreads from human to human.”
Still, until more is known, it says anyone exposed to respiratory tissues and fluids from deer should wear a well-fitting mask and avoid splashing of fluids as much as possible.
COVID-19 has infected multiple species of animals, including dogs, cats, farmed mink and zoo animals. But this is the first time in Canada that it has spilled over into wildlife.
Advertisement
Story continues below
Article content
Deer in the Estrie region of Quebec were sampled Nov. 6 to 8. The National Centre for Foreign Animal Disease confirmed the virus in three of them on Monday. The World Organisation for Animal Health was notified on Wednesday.
“As this is the first detection of SARS-CoV-2 in wildlife in Canada, information on the impacts and spread of the virus in wild deer populations is currently limited,” Environment Canada said in a news release Wednesday.
“This finding emphasizes the importance of ongoing surveillance for SARS-CoV-2 in wildlife to increase our understanding about SARS-CoV-2 on the human-animal interface.”

COVID-19 shows up in Canadian wildlife for first time with three Quebec deer infected
OTTAWA — For the first time, the COVID-19 virus has been detected in Canadian wildlife.